Bronchiectasis
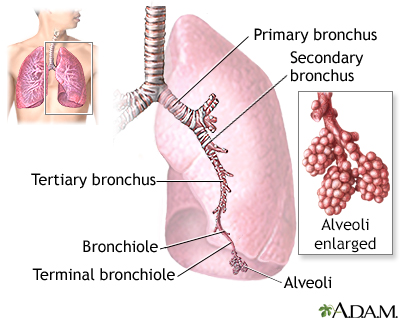
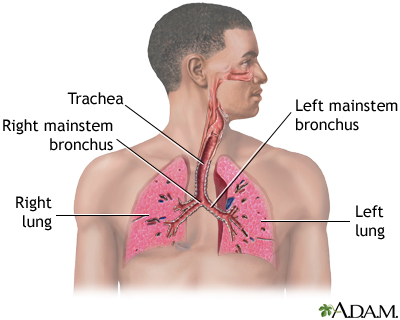
Bronchiectasis is a disease in which the large airways in the lungs are damaged. This causes the airways to become permanently wider.
Bronchiectasis can be present at birth or infancy, which is rare, or develop later in life.
Causes
Bronchiectasis is often caused by inflammation or an infection of the airways that keeps coming back.
Sometimes it begins in childhood after having a severe lung infection or inhaling a foreign object. Breathing in food particles can also lead to this condition.
Inhaling a foreign object
If you swallow a foreign object, it can get stuck in the gastrointestinal (GI) tract from the esophagus (swallowing tube) to the colon (large intesti...
Read Article Now Book Mark ArticleOther causes of bronchiectasis can include:
- Cystic fibrosis, a disease that causes thick, sticky mucus to build up in the lungs
Cystic fibrosis
Cystic fibrosis is a disease that causes thick, sticky mucus to build up in the lungs, digestive tract, and other areas of the body. It is one of th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Autoimmune disorders, such as rheumatoid arthritis, Sjögren syndrome, or inflammatory bowel disease
- Allergic lung diseases
- Leukemia and related cancers
- Immune deficiency syndromes
- Primary ciliary dyskinesia (another congenital disease)
- Infection with non-tuberculous mycobacteria
- As a complication of bronchiolitis obliterans
- Asthma or chronic obstructive lung disease (uncommon)
Symptoms
Symptoms develop over time. They may occur months or years after the event that causes the bronchiectasis.
Long-term (chronic) cough with large amounts of foul smelling sputum is the main symptom of bronchiectasis. Other symptoms may include:
- Breath odor
- Coughing up blood (less common in children)
- Fatigue
- Paleness
Paleness
Paleness is an abnormal loss of color from normal skin or mucous membranes.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Shortness of breath that gets worse with exercise
Shortness of breath
Breathing difficulty may involve:Difficult breathing Uncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Weight loss
- Wheezing
Wheezing
Wheezing is a high-pitched whistling sound during breathing. It occurs when air moves through narrowed breathing tubes in the lungs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Low grade fever and night sweats
- Clubbing of fingers (rare, depends on the cause)
Exams and Tests
Your health care provider will perform a physical exam. When listening to the chest with a stethoscope, your provider may hear small clicking, bubbling, wheezing, rattling, or other sounds, usually in the lower lungs.
Tests that may be done include:
- Aspergillosis precipitin test (to check for signs of an allergic reaction to Aspergillus fungus)
- Alpha-1 antitrypsin blood test
- Chest x-ray
Chest x-ray
A chest x-ray is an x-ray of the chest, lungs, heart, large arteries, ribs, and diaphragm.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Chest CT
- Sputum culture
- Complete blood count (CBC)
Complete blood count
A complete blood count (CBC) test measures the following:The number of white blood cells (WBC count)The number of red blood cells (RBC count)The numb...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Genetic testing, including sweat test for cystic fibrosis and tests for other diseases (like primary ciliary dyskinesia)
Sweat test
Sweat electrolytes is a test that measures the level of chloride in sweat. The sweat chloride test is the standard test used to diagnose cystic fibr...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - PPD skin test to check for a past tuberculosis infection
PPD skin test
The PPD skin test is a method used to diagnose silent (latent) tuberculosis (TB) infection. PPD stands for purified protein derivative.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Serum immunoglobulin electrophoresis to measure proteins called immunoglobulins in the blood
- Lung function tests to measure breathing and how well the lungs are functioning
- Immune deficiency workup
Treatment
Treatment is aimed at:
- Reducing infections and sputum
- Relieving airway blockage
- Preventing the problem from becoming worse
- Treating the underlying cause (for example modulator therapy for people with cystic fibrosis)
Daily drainage to remove sputum is part of treatment. A respiratory therapist can show the person coughing exercises that will help.
Medicines are often prescribed. These include:
- Antibiotics to treat infections
- Bronchodilators to open up airways
- Expectorants to help loosen and cough up thick sputum
Surgery to remove (resect) the lung may be helpful if medicine does not work and the disease is in a small area, or if the person has a lot of bleeding in the lungs. It is more commonly considered if there is no genetic or acquired predisposition to bronchiectasis (for example, more likely to consider if there is bronchiectasis in one segment of the lung only because of prior obstruction).
In severe cases, lung transplantation might be needed.
Outlook (Prognosis)
The outlook depends on the specific cause of the disease. With treatment, most people live without major disability and the disease progresses slowly.
Possible Complications
Complications of bronchiectasis may include:
- Cor pulmonale
- Coughing up blood
- Low oxygen levels (in severe cases)
- Recurrent pneumonia
- Depression
When to Contact a Medical Professional
Contact your provider if:
- You have chest pain or shortness of breath that gets worse
- There is a change in the color or amount of phlegm you cough up, or if it is bloody
- Other symptoms get worse or do not improve with treatment
Prevention
You can reduce your risk by promptly treating lung infections.
Childhood vaccines a yearly flu vaccine, and COVID-19 vaccines help reduce the chance of some infections. Avoiding upper respiratory infections, smoking, and pollution may also reduce your risk of getting this infection.
Vaccines
Vaccines are used to boost your immune system, reduce the risk of infection, and lessen the severity of infections, including those that cause seriou...

Flu vaccine
All content below is taken in its entirety from the CDC Inactivated Influenza Vaccine Information Statement (VIS) www. cdc. gov/vaccines/hcp/current-...

Reviewed By
Allen J. Blaivas, DO, Division of Pulmonary, Critical Care, and Sleep Medicine, VA New Jersey Health Care System, Clinical Assistant Professor, Rutgers New Jersey Medical School, East Orange, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Chang AB, Redding GJ. Bronchiectasis and chronic suppurative lung disease. In: Bush A, Deterding R, Li AM, et al, eds. Kendig and Wilmott's Disorders of the Respiratory Tract in Children. 10th ed. Philadelphia, PA: Elsevier; 2024:chap 44.
O'Donnell AE. Bronchiectasis, atelectasis, and cavitary or cystic lung diseases. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 78.
Solomon GM, Chan ED. Bronchiectasis. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 69.
Disclaimer
© 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.