Causes
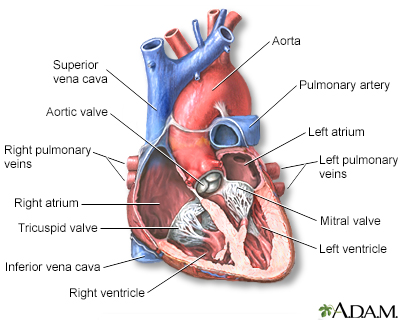
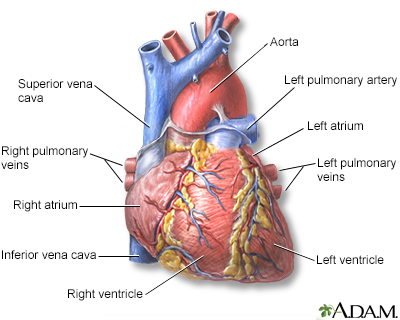
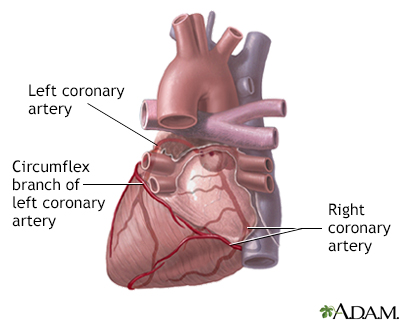
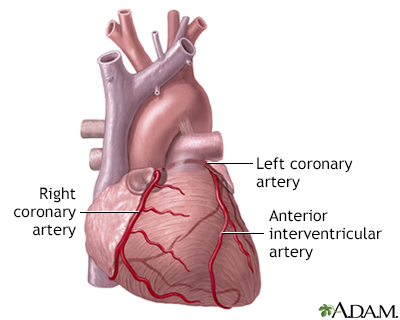
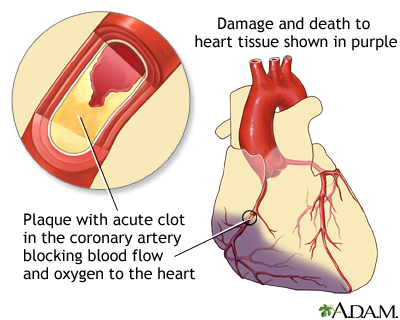
Most heart attacks are caused by a blood clot that blocks one of the coronary arteries. The coronary arteries bring blood and oxygen to the heart. If the blood flow is blocked, the heart is starved of oxygen and heart cells die.
The medical term for this is myocardial infarction.
Acute MI
Causes
A substance called plaque can build up in the walls of your coronary arteries. This plaque is made up of cholesterol and other cells.
A heart attack may occur when:
- A tear in the plaque occurs. This triggers blood platelets and other substances to form a blood clot at the site that blocks most or all of the oxygen-carrying blood from flowing to a part of the heart muscle. This is the most common cause of heart attack.
- A slow buildup of plaque may narrow one of the coronary arteries so that it is almost blocked.
In either case, there is not enough blood flow to the heart muscle and heart muscle dies. PLEASE REVIEW THE ENTIRE ARTICLE
The cause of heart attack is not always known.

Progressive build-up of plaque in coronary artery
Heart attack may occur:
- When you are resting or asleep
- After a sudden increase in physical activity
- When you are active outside in cold weather
- After sudden, severe emotional or physical stress, including an illness
Many risk factors may lead to the development of plaque buildup and a heart attack.
Risk factors may lead to the developmen...
Coronary heart disease (CHD) is a narrowing of the blood vessels that supply blood and oxygen to the heart. CHD is also called coronary artery disea...
Read Article Now Book Mark ArticleVideo Transcript
Heart attack - Animation
Symptoms
A heart attack is a medical emergency. If you have symptoms of a heart attack, call 911 or your local emergency number right away.
- DO NOT try to drive yourself to the hospital.
- DO NOT WAIT. You are at greatest risk of sudden death in the early hours of a heart attack.
Chest pain is the most common symptom of a heart attack.
- You may feel the pain in only one part of your body OR
- Pain may move from your chest to your arms, shoulder, neck, teeth, jaw, belly area, or back
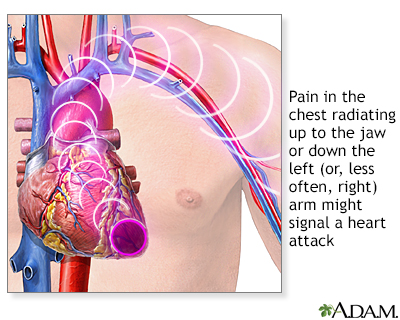
Heart attack symptoms
The pain can be severe or mild. It can feel like:
- A tight band around the chest
- Bad indigestion
- Something heavy sitting on your chest
- Squeezing or heavy pressure
The pain most often lasts longer than 20 minutes. Rest and a medicine to relax the blood vessels (called nitroglycerin) may not completely relieve the pain of a heart attack. Symptoms may also go away and come back.
Other symptoms of a heart attack can include:
- Anxiety
Anxiety
Stress is a feeling of emotional or physical tension. It can come from any event or thought that makes you feel frustrated, angry, or nervous. Stres...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Cough
- Fainting
- Lightheadedness, dizziness
- Nausea and vomiting
- Palpitations (feeling like your heart is beating too fast or irregularly)
- Shortness of breath
- Sweating, which may be very heavy
Some people (the older adults, people with diabetes, and women) may have little or no chest pain. Or, they may have unusual symptoms such as shortness of breath, fatigue, and weakness. A "silent heart attack" is a heart attack with no symptoms.
Exams and Tests
A health care provider will perform a physical exam and listen to your chest using a stethoscope.
- The provider may hear abnormal sounds in your lungs (called crackles), a heart murmur, or other abnormal sounds.
- You may have a fast or uneven pulse.
- Your blood pressure may be normal, high, or low.
You will have an electrocardiogram (ECG) to look for heart damage. Most of the time, certain changes on the ECG indicate you are having a heart attack. Sometimes these changes are not present, even though other tests indicate you have had a heart attack. This can be called non-ST elevation myocardial infarction (NSTEMI).
A blood test can show if you have heart tissue damage. This test can confirm that you are having a heart attack. You will likely have this test 3 times over the first 6 to 12 hours.
Coronary angiography may be done right away or when you are more stable.
- This test uses a special dye and x-rays to see how blood flows through your heart.
- It can help your doctor decide which treatments you need next.
Other tests to look at your heart that may be done while you are in the hospital:
- Echocardiography with or with stress testing
- Exercise stress test
- Nuclear stress test
- Heart CT scan or heart MRI
Treatment
IMMEDIATE TREATMENT
- You will be hooked up to a heart monitor, so the health care team can see how regularly your heart is beating.
- You will receive oxygen so that your heart doesn't have to work as hard.
- An intravenous line (IV) will be placed into one of your veins. Medicines and fluids pass through this IV.
- You may get nitroglycerin and morphine to help reduce chest pain.
- You may receive aspirin, unless it would not be safe for you. In that case, you will be given another medicine that prevents blood clots.
- Dangerous abnormal heartbeats (arrhythmias) may be treated with medicine or electric shocks.
EMERGENCY PROCEDURES
Angioplasty is a procedure to open narrowed or blocked blood vessels that supply blood to the heart.
- Angioplasty is often the first choice of treatment. It should be done within 90 minutes after you get to the hospital, and usually no later than 12 hours after a heart attack.
- A stent is a small, metal mesh tube that opens up (expands) inside a coronary artery. A stent is usually placed after or during angioplasty. It helps prevent the artery from closing up again.
You may be given drugs to break up the clot. This is called thrombolytic therapy. It is best if these drugs are given soon after the onset of symptoms, usually no later than 12 hours after it and ideally within 30 minutes of arriving to the hospital.
Some people may also have heart bypass surgery to open narrowed or blocked blood vessels that supply blood to the heart. This procedure is also called coronary artery bypass grafting and/or open heart surgery.
TREATMENT AFTER A HEART ATTACK
After several days, you will be discharged from the hospital.
You will likely need to take medicines, some for the rest of your life. Always talk to your provider before stopping or changing how you take any medicines. Stopping certain medicines can be deadly.
While under the care of your health care team, you will learn:
- How to take medicines to treat your heart problem and prevent more heart attacks
- How to eat a heart-healthy diet
Heart-healthy diet
A heart-healthy diet is low in saturated fat. Saturated fat can increase your bad cholesterol and clog your arteries. A heart-healthy diet also lim...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - How to be active and exercise safely
- What to do when you have chest pain
- How to stop smoking
Stop smoking
There are many ways to quit smoking. There are also resources to help you. Family members, friends, and co-workers may be supportive. But to be su...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Strong emotions are common after a heart attack.
- You may feel sad
- You may feel anxious and worry about being careful about everything you do
All of these feelings are normal. They go away for most people after 2 or 3 weeks.
You may also feel tired when you leave the hospital to go home.
Most people who have had a heart attack take part in a cardiac rehabilitation program.
Support Groups
Many people benefit from taking part in support groups for people with heart disease.
Support groups for people with heart di...
The following organizations are good resources for information on heart disease:American Heart Association -- www. heart. orgCenters for Disease Cont...

Outlook (Prognosis)
After a heart attack, you have a higher chance of having another heart attack.
How well you do after a heart attack depends on several factors such as:
- The amount of damage to your heart muscle and heart valves
- Where that damage is located
- Your medical care after the heart attack
If your heart can no longer pump blood out to your body as well as it used to, you may develop heart failure. Abnormal heart rhythms can occur, and they can be life threatening.
Heart failure
Heart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptom...

Most people can slowly go back to normal activities after a heart attack. This includes sexual activity. Talk to your provider about how much activity is good for you.
Reviewed By
Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-e228. PMID: 25260718 www.ncbi.nlm.nih.gov/pubmed/25260718.
Anderson JL. ST segment elevation acute myocardial infarction and complications of myocardial infarction. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 73.
Bohula EA, Morrow DA. ST-elevation myocardial infarction: Management. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier; 2019:chap 59.
Giugliano RP, Braunwald E. Non-ST elevation acute coronary syndromes. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier; 2019:chap 60.
O'Gara PT, Kushner FG, Ascheim DD, et al; American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):485-510. PMID: 23256913 www.ncbi.nlm.nih.gov/pubmed/23256913.
Scirica BM, Libby P, Morrow DA. ST-elevation myocardial infarction: pathophysiology and clinical evolution. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier ; 2019:chap 58.