Crohn disease
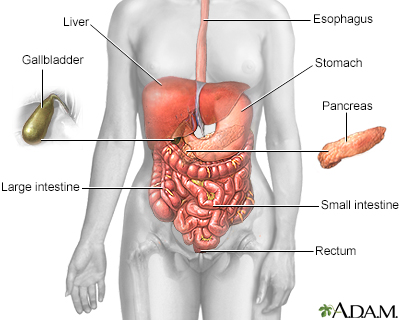
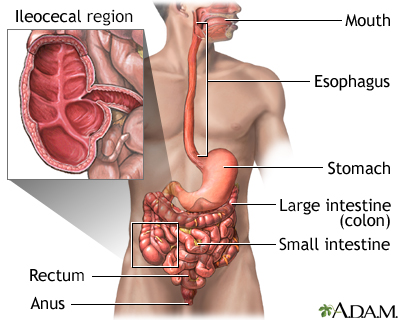
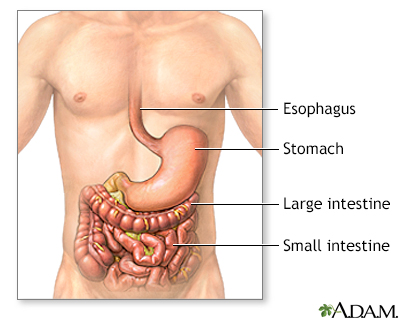
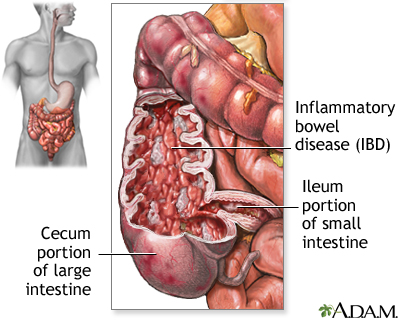
Crohn disease is a disease where parts of the digestive tract become inflamed.
- It most often involves the lower end of the small intestine and the beginning of the large intestine.
- It may also occur in any part of the digestive system from the mouth to the end of the rectum (anus).
Video Transcript
Crohn disease - Animation
Living with Crohn disease can be a constant gamble, hoping this won’t be the day when your disease flares up. Crohn disease is a type of inflammatory bowel disease. It’s caused by a malfunction in the body’s immune system. Normally, the immune system protects against bacteria and other foreign invaders. But in people with Crohn disease, it mistakenly attacks the intestines, causing them to swell up and thicken. As a result, people with Crohn disease have bouts of severe abdominal pain, diarrhea, and pain with bowel movements. They can lose their appetite, feel tired, and lose weight without meaning to. Some have severe mouth sores. If you’ve been experiencing any of these symptoms, your doctor can test for Crohn with a colonoscopy using a scope to look at your colon from the inside. A wireless video capsule may be swallowed to look at the small intestines. Blood tests or other imaging studies may be needed as well. If you’re concerned about Crohn's, stop smoking. Smoking can increase your chance of getting Crohn disease and once you have it smoking can make the condition worse. Medicines can help with the symptoms of Crohn disease. There are medicines to control diarrhea, and pain relievers to help with abdominal cramps. There are also medicines that quiet the overactive immune response that causes Crohn. Changing your diet may make a big difference in preventing or reducing symptoms. But the diet that works well for you may be different than the one that works for others. Eating several small meals a day instead of three big ones prevents your intestines from having to process large amounts of food at once. Your doctor may also recommend that you drink lots of water, and avoid high-fiber and high-fatty foods, as well as any foods that you know make you gassy, perhaps beans or broccoli. You may also need to take iron, B12, and other vitamin and mineral supplements if your Crohn is preventing you from getting enough nutrients through your diet. If medicines and diet changes aren’t enough to reduce your symptoms, and you develop bleeding or an infection in your intestines, you may need a procedure called a bowel resection to remove the diseased part of your intestines. This procedure won’t cure Crohn, but it can help control the complications of the disease. If you’re experiencing Crohn symptoms, like stomach pain, severe diarrhea, or unplanned weight loss, call your doctor. Although there’s no cure for Crohn, treatments can relieve some of the uncomfortable symptoms, prevent complications, helping improve your quality of life.
Crohn disease is a form of inflammatory bowel disease (IBD).
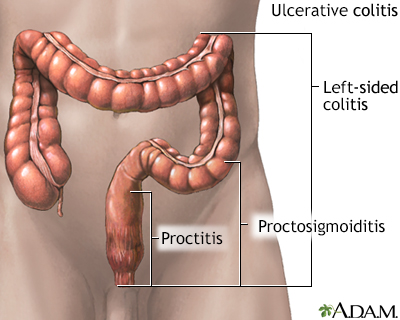
Ulcerative colitis is another form of IBD.
Ulcerative colitis
Ulcerative colitis is a condition in which the lining of the large intestine (colon) and rectum become inflamed. It is a form of inflammatory bowel ...

Inflammatory bowel disease
Crohn disease, also called regional enteritis, is a chronic inflammation of the intestines which is usually confined to the terminal portion of the small intestine, the ileum. Ulcerative colitis is a similar inflammation of the colon, or large intestine. These and other IBDs (inflammatory bowel disease) have been linked with an increased risk of colorectal cancer.
Causes
The exact cause of Crohn disease is unknown. It occurs when your body's immune system mistakenly attacks and destroys healthy body tissue (autoimmune disorder), mainly in the digestive tract.
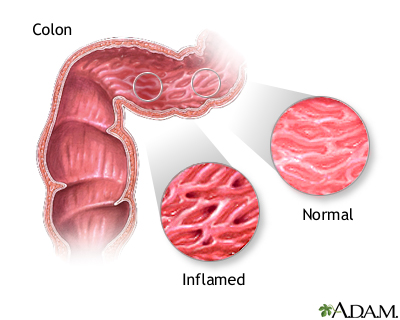
When parts of the digestive tract remain swollen or inflamed, the walls of the intestines become thickened.
Factors that may play a role in Crohn disease include:
- Your genes and family history. (People who are white or of Eastern European Jewish descent are at a higher risk. But the risk has been rising in many different groups.)
- Environmental factors.
- Tendency of your body to overreact to normal bacteria in the intestines.
- Smoking.
Crohn disease may occur at any age. It mostly begins in people between ages 15 and 35. But recently Crohn disease has been increasing in the older population, too.
Symptoms
Symptoms depend on the part of the digestive tract involved. Symptoms range from mild to severe, and can come and go, with periods of flare-ups.
The main symptoms of Crohn disease are:
- Crampy pain in the abdomen (belly area).
- Fever.
- Fatigue.
- Loss of appetite and weight loss.
- Feeling that you need to pass stools, even though your bowels are already empty (tenesmus). It may involve straining, pain, and cramping.
- Watery or loose diarrhea, which may be bloody.
Other symptoms may include:
- Constipation
- Sores or swelling in the eyes
- Draining of pus, mucus, or stools from around the rectum or anus (caused by an abnormal opening in the skin called a fistula)
- Joint pain and swelling
- Mouth ulcers
- Rectal bleeding and bloody stools
Bloody stools
Black or tarry stools with a foul smell are a sign of a problem in the upper digestive tract. It most often indicates that there is bleeding in the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Swollen gums
- Tender, red bumps (nodules) under the skin, which may turn into skin ulcers

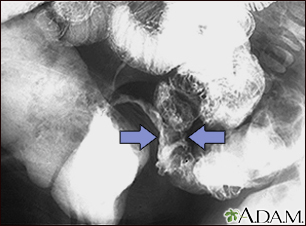
Anorectal fistulas
Crohn disease is an inflammation of the intestines caused by immune response to an infection. The lining of the intestine may ulcerate and form channels of infection, called fistulas. Fistulas tunnel from the area of ulceration, creating a hole which may continue until it reaches the surface of the organ, or the surface of nearby skin. These holes typically spread the infection that creates them, and life-threatening conditions such as peritonitis (inflammation of the lining of the abdomen) may occur.
Exams and Tests
A physical exam may show a mass or tenderness in the abdomen, skin rash, swollen joints, or mouth ulcers.
Tests to diagnose Crohn disease include:
- Barium enema or upper GI (gastrointestinal) series
- Colonoscopy or sigmoidoscopy (often done with a biopsy)
- CT scan of the abdomen
- Capsule endoscopy
- MRI of the abdomen
- Enteroscopy
- MR enterography or CT enterography
A stool culture or other tests may be done to check for other possible causes of the symptoms, such as infection, and to look for inflammation.
This disease may also alter the results of the following tests:
- Low albumin level
- High erythrocyte sedimentation rate
- Elevated C-reactive protein (CRP)
- Fecal fat
- Low blood count (hemoglobin and hematocrit)
- Abnormal liver blood tests
- High white blood cell count
- Elevated fecal calprotectin level in stool
Treatment
Tips for managing Crohn disease at home:
DIET AND NUTRITION
You should eat a well-balanced, healthy diet. Include enough calories, protein, and nutrients from a variety of food groups.
An elemental diet has been shown to improve Crohn disease and its symptoms. However, this diet is not used often because of the taste.
Depending on the location(s) of your Crohn disease, the type of your Crohn disease, and the other problems it may cause, certain foods may be more difficult to eat. Types of food problems may vary from person to person.
Some foods can make diarrhea and gas worse. To help ease symptoms, try:
- Eating small amounts of food throughout the day.
- Drinking lots of water (drink small amounts often throughout the day).
- Avoiding high-fiber foods (bran, beans, nuts, seeds, and popcorn).
- Avoiding large amounts of uncooked or fibrous vegetables and fruits. Sometimes peeling, softening, or pureeing helps.
- Avoiding fatty, greasy, or fried foods and sauces (butter, margarine, and heavy cream).
- Limiting dairy products if you have problems digesting dairy fats. Try low-lactose cheeses, such as Swiss and cheddar, and an enzyme product, such as Lactaid, to help break down lactose.
- Avoiding foods that you know cause gas, such as beans and vegetables in the cabbage family, such as broccoli.
- Avoiding spicy foods.
Ask your health care provider about extra vitamins and minerals you may need, such as:
- Iron supplements (if you are iron deficient).
- Calcium and vitamin D supplements to help keep your bones strong.
- Vitamin B12 to prevent anemia, especially if you have had the end of the small intestine (ileum) removed.
If you have an ileostomy, you will need to learn:
- Diet changes
- How to change your pouch
- How to care for your stoma
STRESS
You may feel worried, embarrassed, or even sad and depressed about having a bowel disease. Other stressful events in your life, such as moving, a job loss, or the loss of a loved one can worsen digestive problems.
Ask your provider for tips on how to manage your stress.
MEDICINES
Ask your provider about taking anti-diarrheal medicines. In general, these should be avoided in people with IBD, if possible. Treating the IBD is the key to making diarrhea and other symptoms better.
Other medicines to help with symptoms include:
- Fiber supplements, such as psyllium powder (Metamucil) or methylcellulose (Citrucel). Ask your provider before taking these products or laxatives.
- Acetaminophen (Tylenol) for mild pain. Avoid medicines such as aspirin, ibuprofen (Advil, Motrin), or naproxen (Aleve, Naprosyn) which can make your symptoms worse.
Your provider may also prescribe medicines to help control Crohn disease:
- Aminosalicylates (5-ASAs) are medicines that help control mild to moderate symptoms. Some forms of the medicine are taken by mouth, and others must be given rectally. The latter are only used in Crohn disease of the large intestine.
- Corticosteroids, such as prednisone or budesonide, treat moderate to severe Crohn disease. They may be taken by mouth or inserted into the rectum. They may help until a long-term medicine with fewer side effects is started and can take effect.
- Antibiotics to treat abscesses or fistulas.
- Immunosuppressive medicines that quiet the immune system's reaction such as azathioprine, 6-mercaptopurine, and others to avoid long-term use of corticosteroids.
- Biologic therapy and small molecule therapy are the most common long-term treatments. They are given in different ways (oral, injection, infusion). Speak with your provider about your particular situation.
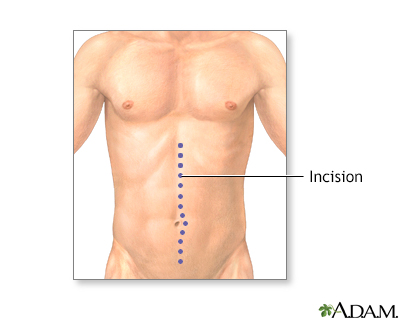
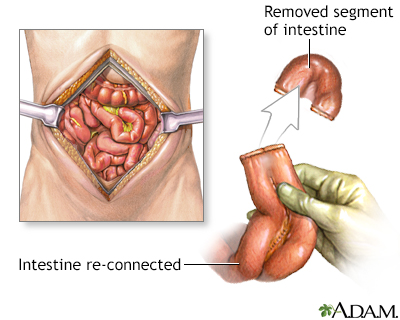
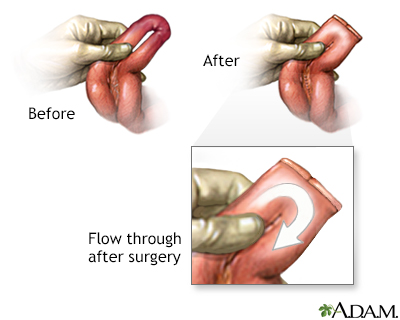
SURGERY
Some people with Crohn disease may need surgery to remove a damaged or diseased part of the intestine. In some cases, the entire large intestine is removed, with or without the rectum.
People who have Crohn disease that does not respond to medicines may need surgery to treat problems such as:
- Bleeding
- Failure to grow (in children)
- Fistulas (abnormal connections between the intestines and another area of the body)
- Infections
- Narrowing of the intestine (strictures)
Surgeries that may be done include:
- Ileostomy
- Removal of part of the large bowel or small bowel
- Removal of the large intestine to the rectum
- Removal of the large intestine and most of the rectum
Support Groups
Social support can often help with the stress of dealing with illness, and support group members may also have useful tips for finding the best treatment and coping with the condition.
More information and support for people with Crohn disease and their families can be found at:
Outlook (Prognosis)
There is no cure for Crohn disease. However, the goals of treatment are to quiet the disease and keep it quiet. Surgery is used in particular situations but does not cure Crohn disease. If you smoke, stopping will help improve the disease.
Possible Complications
You have more risk for small bowel and colon cancer if you have Crohn disease. Your provider may suggest tests to screen for colon cancer. A colonoscopy is often recommended if you have had Crohn disease involving the colon for 8 or more years.
Those with more severe Crohn disease may have these problems:
- Abscess or infection in the intestines
- Anemia, a lack of red blood cells
- Bowel blockage
- Fistulas in the bladder, skin, or vagina
- Slow growth and sexual development in children
- Swelling of the joints
- Lack of important nutrients, such as vitamin B12 and iron
- Problems with maintaining a healthy weight
- Inflammation of the bile ducts (primary sclerosing cholangitis)
- Skin lesions, such as pyoderma gangrenosum
When to Contact a Medical Professional
Contact your provider if you:
- Have very bad abdominal pain
- Cannot control your diarrhea with diet changes and medicines
- Have lost weight, or your child with Crohn disease is not gaining weight
- Have rectal bleeding, drainage, or sores
- Have a fever that lasts for more than 2 or 3 days, or a fever higher than 100.4°F (38°C) without an illness
- Have nausea and vomiting that lasts for more than a day
- Have skin sores that do not heal
- Have joint pain that prevents you from doing your everyday activities
- Have side effects from medicines you are taking for your condition
Reviewed By
Jenifer K. Lehrer, MD, Gastroenterologist, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Ananthakrishnan AN, Reguerio MD. Management of inflammatory bowel diseases. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 116.
Feuerstein JD, Ho EY; American Gastroenterological Association Institute Clinical Guidelines Committee, et al. AGA clinical practice guidelines on the medical management of moderate to severe luminal and perianal fistulizing Crohn's disease. Gastroenterology. 2021;160(7):2496-2508. PMID: 34051983 pubmed.ncbi.nlm.nih.gov/34051983/.
Galandiuk S, Netz U, Morpurgo E, Tosato SM, Abu-Freha N, Ellis CT. Colon and rectum. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 52.
Kaplan GG, Ng SC. Epidemiology, pathogenesis, and diagnosis of inflammatory bowel diseases. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 115.
Lichtenstein GR. Inflammatory bowel disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 127.
Ricci JP, Talamini MA. Management of Crohn's disease of the small bowel. In: Cameron J, ed. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:134-137.
Disclaimer
© 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.