Cirrhosis
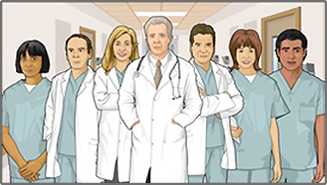
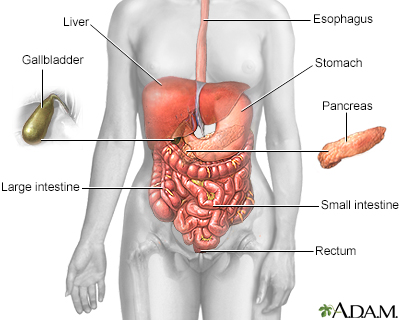
Cirrhosis is scarring of the liver and poor liver function. It is the last stage of chronic liver disease.
Causes
Cirrhosis is most often the end result of chronic liver damage caused by long-term (chronic) liver disease. Common causes of chronic liver disease in the United States are:
- Hepatitis B or hepatitis C infection.
- Alcohol overuse.
- Buildup of fat in the liver that is NOT caused by drinking too much alcohol (called metabolic associated steatotic liver disease [MASLD] or metabolic associated steatohepatitis [MASH]). It is closely related to being overweight, having high blood pressure, diabetes or pre-diabetes, and high cholesterol.
Less common causes of cirrhosis include:
- When immune cells mistake the liver's normal cells for harmful invaders and attack them, called autoimmune hepatitis (AH)
- Bile duct disorders
- Some medicines
- Liver diseases passed down in families
Symptoms
There may be no symptoms, or symptoms may come on slowly, depending on how well the liver is working. Often, it is discovered by chance when an abdominal ultrasound exam is done or blood is drawn for another reason.
Early symptoms include:
- Fatigue and loss of energy
- Poor appetite and weight loss
- Nausea or belly pain
- Small, red spider-like blood vessels on the skin
As liver function worsens, symptoms may include:
- Fluid buildup in the legs (edema) and in the abdomen (ascites)
- Yellow color in the skin, mucous membranes, or eyes (jaundice)
- Redness on the palms of the hands
- In men, impotence, shrinking of the testicles, and breast swelling
- Easy bruising and abnormal bleeding, most often from swollen veins in the digestive tract
- Confusion or problems thinking
- Pale or clay-colored stools
- Bleeding from upper or lower gastrointestinal tract
Exams and Tests
Your health care provider will do a physical exam to look for:
- An enlarged liver or spleen
- Excess breast tissue (in men)
- Swollen abdomen, as a result of too much fluid
Swollen abdomen
Ascites is the build-up of fluid in the space between the lining of the abdomen and abdominal organs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Reddened palms
- Red spider-like blood vessels on the skin
- Small testicles (in men)
- Widened veins in the abdomen wall
- Yellow eyes or skin (jaundice)
You may have the following tests to determine the cause of your cirrhosis:
- Hepatitis virus testing
- Antibody testing for autoimmune hepatitis
- Serum iron saturation and ferritin levels
- Serum ceruloplasmin level
- Genetic testing for liver disorders
You may have the following tests to measure liver function:
- Complete blood count
Complete blood count
A complete blood count (CBC) test measures the following:The number of white blood cells (WBC count)The number of red blood cells (RBC count)The numb...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Prothrombin time
Prothrombin time
Liver function tests are common tests that are used to see how well the liver is working. Tests include:AlbuminAlpha-1 antitrypsinAlkaline phosphata...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Liver function tests
Liver function tests
Liver function tests are common tests that are used to see how well the liver is working. Tests include:AlbuminAlpha-1 antitrypsinAlkaline phosphata...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Blood albumin level
Other tests to check for liver damage include:
- Computed tomography (CT) of the abdomen
Computed tomography (CT) of the abdomen
An abdominal CT scan is an imaging test that uses x-rays to create cross-sectional pictures of the belly area. CT stands for computed tomography....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Magnetic resonance imaging (MRI) of the abdomen
Magnetic resonance imaging (MRI) of the...
An abdominal magnetic resonance imaging scan is an imaging test that uses powerful magnets and radio waves. The waves create pictures of the inside ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Endoscopy to check for abnormal veins in the esophagus or stomach
Endoscopy
Endoscopy is a way of looking inside the body using a flexible tube that has a small camera and light on the end of it. This instrument is called an...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Ultrasound of the abdomen
You might need a liver biopsy to confirm the diagnosis.
Liver biopsy
A liver biopsy is a test that takes a sample of tissue from the liver for examination.

Treatment
LIFESTYLE CHANGES
Some things you can do to help take care of your liver disease are:
- Drink no alcohol.
- Eat a healthy diet that is low in salt, fat, and simple carbohydrates.
- Get vaccinated for diseases such as influenza, COVID-19, hepatitis A and B, and pneumococcal disease.
- Talk to your provider about all medicines you take, including herbs and supplements and over-the-counter medicines.
- Exercise.
- Control your underlying metabolic problems, such as high blood pressure, diabetes, and high cholesterol.
MEDICINES FROM YOUR PROVIDER
- Water pills (diuretics) to get rid of fluid build-up.
- Vitamin K or blood products to prevent excess bleeding.
- Medicines for mental confusion.
- Antibiotics for infections.
- Medicines to cure Hepatitis C.
- Medicines to cure Hepatitis B.
- New medicines are being created to treat MASH. One was just FDA approved, called resmetirom (Rezdiffra) Your doctor can discuss whether you should be treated with this medicine.
OTHER TREATMENTS
- Endoscopic treatments for enlarged veins in the esophagus (varices)
- Removal of fluid from the abdomen (paracentesis)
- Placement of a transjugular intrahepatic portosystemic shunt (TIPS) to improve blood flow in the liver
When cirrhosis progresses to end-stage liver disease, a liver transplant may be needed.
Support Groups
You can often ease the stress of illness by joining a liver disease support group whose members share common experiences and problems.
Outlook (Prognosis)
Cirrhosis is caused by scarring of the liver. In most cases, the liver cannot heal or return to normal function once the damage is severe. Cirrhosis can lead to serious complications.
Possible Complications
Complications may include:
- Bleeding disorders
- Buildup of fluid in the abdomen (ascites) and infection of the fluid (spontaneous bacterial peritonitis)
- Enlarged veins in the esophagus, stomach, or intestines that bleed easily (varices)
- Increased pressure in the blood vessels of the liver (portal hypertension)
- Kidney failure (hepatorenal syndrome)
- Liver cancer (hepatocellular carcinoma)
Hepatocellular carcinoma
Hepatocellular carcinoma is cancer that starts in the liver.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Mental confusion, change in the level of consciousness, or coma (hepatic encephalopathy)
When to Contact a Medical Professional
Contact your provider if you develop symptoms of cirrhosis.
Get emergency medical help right away if you have:
- Abdominal or chest pain
- Abdominal swelling or ascites that is new or suddenly becomes worse
- A fever (temperature greater than 101°F or 38.3°C)
- Diarrhea
- Confusion or a change in alertness, or it gets worse
- Rectal bleeding, vomiting blood, or blood in the urine
- Shortness of breath
- Vomiting more than once a day
- Yellowing skin or eyes (jaundice) that is new or gets worse quickly
Prevention
DO NOT drink alcohol. Talk to your provider if you are worried about your drinking. Take steps to prevent getting hepatitis B or C or passing it to other people.
Reviewed By
Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
FDA News Release. FDA approves first treatment for patients with liver scarring due to fatty liver disease. March 14, 2024. www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-patients-liver-scarring-due-fatty-liver-disease. Accessed July 30, 2024.
Garcia-Tsao G. Cirrhosis and its sequelae. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 139.
Kamath PS, Shah VH. Overview of cirrhosis. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 74.
Rinella ME, Lazarus JV, Ratziu V, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J Hepatol. 2023;79(6):1542-1556. PMID: 37354790 pubmed.ncbi.nlm.nih.gov/37364790/.
Disclaimer
© 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.