Pheochromocytoma
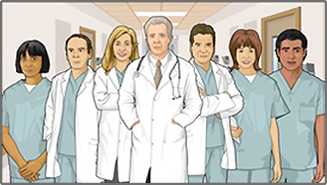
Pheochromocytoma is a rare tumor of adrenal gland tissue that typically arises from the adrenal gland. It results in the release of too much epinephrine and norepinephrine, which are hormones that control heart rate, metabolism, and blood pressure.
Tumor
A tumor is an abnormal growth of body tissue. Tumors can be cancerous (malignant) or noncancerous (benign).
Read Article Now Book Mark ArticleCauses
Pheochromocytoma may occur as a single tumor or as more than one growth. It usually develops in the center (medulla) of one or both adrenal glands. The adrenal glands are two triangle-shaped glands. One gland is located on top of each kidney. In rare cases, a pheochromocytoma occurs outside the adrenal gland. When it does, it is usually somewhere else in the abdomen.
Very few pheochromocytomas are cancerous.
The tumors may occur at any age, but they are most common from early to mid-adulthood.
In few instances, the condition may also be seen among family members (hereditary).
Symptoms
Most people with this tumor have attacks of a set of symptoms, which happen when the tumor releases hormones. The attacks usually last from a few minutes to hours. The set of symptoms include:
- Headaches
Headaches
A headache is pain or discomfort in the head, scalp, or neck. Serious causes of headaches are rare. Most people with headaches can feel much better...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Heart palpitations
- Sweating
- High blood pressure
As the tumor grows, the attacks often increase in frequency, length, and severity.
Other symptoms that may occur include:
- Abdominal or chest pain
Abdominal
Abdominal pain is pain that you feel anywhere between your chest and groin. This is often referred to as the stomach region or belly.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleChest pain
Chest pain is discomfort or pain that you feel anywhere along the front of your body between your neck and upper abdomen.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Irritability, nervousness
- Pallor
- Weight loss
Weight loss
Unexplained weight loss is a decrease in body weight, when you did not try to lose the weight on your own. Many people gain and lose weight. Uninten...
Read Article Now Book Mark Article - Nausea and vomiting
- Shortness of breath
- Seizures
Seizures
A seizure is the physical changes in behavior that occurs during an episode of specific types of abnormal electrical activity in the brain. The term ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Problems sleeping
Exams and Tests
Your health care provider will perform a physical exam. You'll be asked about your medical history and symptoms.
Tests done may include:
- Abdominal CT scan
Abdominal CT scan
An abdominal CT scan is an imaging test that uses x-rays to create cross-sectional pictures of the belly area. CT stands for computed tomography....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Adrenal gland biopsy
Adrenal gland biopsy
A biopsy is the removal of a small piece of tissue for lab examination.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Catecholamines blood test (serum catecholamines)
- Glucose test
- Metanephrine blood test (serum metanephrine)
- An imaging test called an MIBG scintiscan
MIBG scintiscan
An MIBG scintiscan is a type of imaging test. It uses a radioactive substance called a tracer injected into your body. A subsequent scan can find o...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - MRI of abdomen
MRI of abdomen
An abdominal magnetic resonance imaging scan is an imaging test that uses powerful magnets and radio waves. The waves create pictures of the inside ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Urine catecholamines
- Urine metanephrines
- PET scan of abdomen
- Bone scan
Treatment
Treatment involves removing the tumor with surgery. It is important to stabilize your blood pressure and pulse with certain medicines before surgery. You may need to stay in the hospital and have your vital signs closely monitored around the time of surgery. After surgery, your vital signs will be continuously monitored in an intensive care unit.
When the tumor cannot be surgically removed, you will need to take medicine to manage it. A combination of medicines is usually needed to control the effects of the extra hormones. Radiation therapy and chemotherapy won't cure this kind of tumor, but they may help control the disease and treat symptoms that arise.
Radiation therapy
Radiation therapy uses high-powered radiation (such as x-rays or gamma rays), particles, or radioactive seeds to kill cancer cells.

Chemotherapy
The term chemotherapy is used to describe cancer-killing drugs. Chemotherapy may be used to:Cure the cancerShrink the cancerPrevent the cancer from ...

Outlook (Prognosis)
Most people who have noncancerous tumors that are removed with surgery are still alive after 5 years. The tumors come back in some people. Levels of the hormones norepinephrine and epinephrine return to normal after surgery.
Continued high blood pressure may occur after surgery. Standard treatments can usually control the high blood pressure.
People who have been successfully treated for pheochromocytoma should have testing from time to time to make sure the tumor has not returned. Close family members may also benefit from testing, because some cases are inherited.
When to Contact a Medical Professional
Contact your provider if you:
- Have symptoms of pheochromocytoma, such as headache, sweating, and palpitations
- Had a pheochromocytoma in the past and your symptoms return
Reviewed By
Warren Brenner, MD, Oncologist, Lynn Cancer Institute, Boca Raton, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 02/24/2025.
Cameron J. Endocrine glands. In: Cameron AM, Cameron JL, eds. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:Sect 13, 809-894.
National Cancer Institute website. Pheochromocytoma and paraganglioma treatment (PDQ) - health professional version. www.cancer.gov/types/pheochromocytoma/hp/pheochromocytoma-treatment-pdq#link/_38_toc. Updated November 1, 2024. Accessed February 24, 2025.
Pacak K, Timmers HJLM, Taieb D, Lenders JWM, Eisenhofer G. Pheochromocytoma. In: Robertson RP, Giudice LC, Grossman AB, Hammer GD, Jensen MD, Kahaly GJ, et al, eds. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 99.
Disclaimer
© 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.