Multimedia Gallery




Knee joint replacement - series
Knee joint replacement - Series
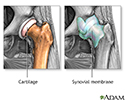
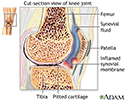
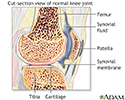
The knee is a complex joint. It contains the distal end of the femur (the femoral condyles) and the proximal end of the tibia (the tibial plateau). The femoral condyles usually glide smoothly on the tibial plateau. This allows the lower leg to move smoothly and painlessly.
Knee joint replacement - series
Knee joint replacement - Series
The knee is a complex joint. It contains the distal end of the femur (the femoral condyles) and the proximal end of the tibia (the tibial plateau). T...
Knee joint replacement - series
Indications
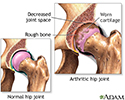
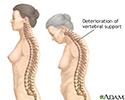
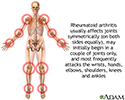
The most common cause of knee damage that leads to knee replacement is osteoarthritis. Osteoarthritis is a degenerative disease of the bones of the knee. It causes the surfaces of the knee joint to become irregular and rough, preventing smooth painless motion of the knee joint.
Knee joint replacement may be recommended for:
- Knee osteoarthritis, or arthritis, which causes knee pain that has failed to respond to conservative therapy (NSAID medication for 6 months or more)
- Decreased knee function caused by arthritis
- Inability to work because of knee pain
- Inability to sleep through the night because of knee pain
- Inability to walk more than 3 blocks because of knee pain
- Loose knee prosthesis
- Some knee fractures
Knee joint replacement - series
Indications
The most common cause of knee damage that leads to knee replacement is osteoarthritis. Osteoarthritis is a degenerative disease of the bones of the k...
Knee joint replacement - series
Procedure
The operation is performed under general anesthesia. The orthopedic surgeon makes an incision over the affected knee. The patella (knee cap) is moved out of the way, and the surgeon shaves the heads of the femur and tibia to remove any rough parts. This allows helps the prosthesis to adhere better. The two parts of the prosthesis are implanted into the thigh bone and the tibia bone using a special bone cement.
Knee joint replacement - series
Procedure
The operation is performed under general anesthesia. The orthopedic surgeon makes an incision over the affected knee. The patella (knee cap) is moved...
Knee joint replacement - series
Aftercare
You will return from surgery with a large dressing on the knee area. A small drainage tube will be placed during surgery to help drain excess fluids from the joint area. Your leg will be placed in a continuous passive motion (CPM) device. This mechanical device that flexes (bends) and extends (straightens) the knee at a pre-set rate and amount of bending.
Gradually, the rate and amount of bending will be increased as you can tolerate it. The leg should always be in this device when you are in bed. The CPM device helps speed recovery, and decreases pain, bleeding, and infection after the operation.
You will have some pain after surgery. However, you may receive intravenous (IV) medicine to control your pain for the first 3 days after surgery. The pain should gradually get better. By the third day after surgery, medicine you take by mouth may be enough to control your pain.
You will also return from surgery with several IV lines in place to give you hydration and nutrition. The IV will be removed when you can drink enough fluids on your own.
You will receive antibiotics to reduce the risk of developing an infection.
You will also return from surgery wearing special stockings. These devices help lower your risk of getting blood clots, which are more common after lower leg surgery.
You will be asked to start moving and walking early after surgery. You will be helped out of bed to a chair on the first day. When in bed, bend and straighten your ankles often. This can prevent blood clots from forming.
Knee joint replacement - series
Aftercare
You will return from surgery with a large dressing on the knee area. A small drainage tube will be placed during surgery to help drain excess fluids ...
Review Date: 6/4/2025
Reviewed By: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
© 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
The knee is a complex joint. It contains the distal end of the femur (the femoral condyles) and the proximal end of the tibia (the tibial plateau). The femoral condyles usually glide smoothly on the tibial plateau. This allows the lower leg to move smoothly and painlessly.
The most common cause of knee damage that leads to knee replacement is osteoarthritis. Osteoarthritis is a degenerative disease of the bones of the knee. It causes the surfaces of the knee joint to become irregular and rough, preventing smooth painless motion of the knee joint.
Knee joint replacement may be recommended for:
- Knee osteoarthritis, or arthritis, which causes knee pain that has failed to respond to conservative therapy (NSAID medication for 6 months or more)
- Decreased knee function caused by arthritis
- Inability to work because of knee pain
- Inability to sleep through the night because of knee pain
- Inability to walk more than 3 blocks because of knee pain
- Loose knee prosthesis
- Some knee fractures
The operation is performed under general anesthesia. The orthopedic surgeon makes an incision over the affected knee. The patella (knee cap) is moved out of the way, and the surgeon shaves the heads of the femur and tibia to remove any rough parts. This allows helps the prosthesis to adhere better. The two parts of the prosthesis are implanted into the thigh bone and the tibia bone using a special bone cement.
You will return from surgery with a large dressing on the knee area. A small drainage tube will be placed during surgery to help drain excess fluids from the joint area. Your leg will be placed in a continuous passive motion (CPM) device. This mechanical device that flexes (bends) and extends (straightens) the knee at a pre-set rate and amount of bending.
Gradually, the rate and amount of bending will be increased as you can tolerate it. The leg should always be in this device when you are in bed. The CPM device helps speed recovery, and decreases pain, bleeding, and infection after the operation.
You will have some pain after surgery. However, you may receive intravenous (IV) medicine to control your pain for the first 3 days after surgery. The pain should gradually get better. By the third day after surgery, medicine you take by mouth may be enough to control your pain.
You will also return from surgery with several IV lines in place to give you hydration and nutrition. The IV will be removed when you can drink enough fluids on your own.
You will receive antibiotics to reduce the risk of developing an infection.
You will also return from surgery wearing special stockings. These devices help lower your risk of getting blood clots, which are more common after lower leg surgery.
You will be asked to start moving and walking early after surgery. You will be helped out of bed to a chair on the first day. When in bed, bend and straighten your ankles often. This can prevent blood clots from forming.




Animations
- Ankle ligament injury
- Ankylosing spondylitis
- Anterior shoulder stretch
- Arm reach
- Arthritis
- Bone fracture repair
- Bunion
- Carpal tunnel syndrome
- Exercise
- External rotation with band
- Fibromyalgia
- Foot pain
- Heel pain
- Herniated disk
- Herniated nucleus pulposus ...
- Hip joint replacement
- How to use a pill cutter
- Internal rotation with band
- Isometric
- Knee joint replacement
- Multiple sclerosis
- Neck pain
- Osteoarthritis
- Osteoarthritis
- Osteoporosis
- Osteoporosis
- Pendulum exercise
- Plantar fasciitis
- Rheumatoid arthritis
- Rotator cuff problems
- Sciatica
- Scoliosis
- Shoulder blade retraction
- Shoulder blade retraction w...
- Shoulder joint dislocation
- Shoulder pain
- Spinal stenosis
- Stretching back of your shoulder
- Up the back stretch
- Vacation health care
- Wall push-up
- Wall stretch
- What is tennis elbow?
Illustrations
- ACL degrees
- ACL injury
- Active vs. inactive muscle
- Aerobic exercise
- Ankle anatomy
- Ankle sprain
- Ankle sprain swelling
- Anterior cruciate ligament ...
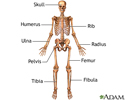
- Anterior skeletal anatomy
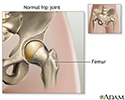
- Arthritis in hip
- Aseptic necrosis
- Baker cyst
- Benefit of regular exercise
- Blood supply to bone
- Blood test
- Bone biopsy
- Bone density scan
- Bone graft harvest
- Bone tumor
- Bone-building exercise
- Bursa of the elbow
- Bursa of the knee
- Bursitis of the shoulder
- Calcium benefit
- Calcium source
- Calculating body frame size
- Calories and fat per serving
- Carpal biopsy
- Carpal tunnel surgical procedure
- Carpal tunnel syndrome
- Cauda equina
- Central nervous system
- Central nervous system and ...
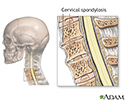
- Cervical spondylosis
- Cervical vertebrae
- Changes in spine with age
- Chest stretch
- Chondromalacia of the patella
- Clubfoot deformity
- Colles fracture
- Common peroneal nerve dysfu...
- Compression fracture
- Compression of the median nerve
- Congenital hip dislocation
- Contracture deformity
- Corns and calluses
- CREST syndrome
- CT scan
- Damaged axillary nerve
- Dislocation of the hip
- Early treatment of injury
- Elbow - side view
- Electromyography
- Ewing sarcoma - x-ray
- Exercise - a powerful tool
- Exercise and age
- Exercise and heart rate
- Exercise can lower blood pr...
- Exercise with friends
- External fixation device
- Fast food
- Femoral fracture
- Femoral nerve damage
- Fibromyalgia
- Fish in diet
- Foot swelling
- Forward bend test
- Fracture types (1)
- Fracture types (2)
- Fracture, forearm - x-ray
- Fractures across a growth plate
- Groin stretch
- Hammer toe
- Hamstring stretch
- Head trauma
- Healthy diet
- Herniated disk repair
- Herniated lumbar disk
- Herniated nucleus pulposus
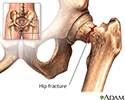
- Hip fracture
- Hip stretch
- Hunger center in brain
- Hypermobile joints
- Impingement syndrome
- Inflamed Achilles tendon
- Inflamed shoulder tendons
- Internal fixation devices
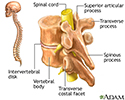
- Intervertebral disk
- Isometric exercise
- Joint aspiration
- Knee arthroscopy
- Knee joint
- Knee joint replacement pros...
- Knee pain
- Kyphosis
- Lateral collateral ligament
- Lateral collateral ligament...
- Lateral collateral ligament pain
- Leg pain (Osgood-Schlatter)
- Leg skeletal anatomy
- Limited range of motion
- Location of whiplash pain
- Lordosis
- Lower leg edema
- Lower leg muscles
- Lower leg muscles
- Lumbar vertebrae
- Lupus - discoid on a child'...
- Lupus - discoid on the face
- Lupus, discoid - view of l...
- Medial collateral ligament
- Medial collateral ligament ...
- Medial collateral ligament pain
- Meniscal tears
- Metatarsus adductus
- MRI scans
- Muscle biopsy
- Muscle cells vs. fat cells
- Muscle pain
- Muscle strain
- Muscular atrophy
- myPlate
- Neck pain
- Nerve biopsy
- Nerve conduction test
- Normal foot x-ray
- Normal knee anatomy
- Nuclear scan
- Osteoarthritis
- Osteoarthritis
- Osteoarthritis vs. rheumato...
- Osteogenic sarcoma - x-ray
- Osteomyelitis
- Osteoporosis
- Osteoporosis
- Patellar dislocation
- Physical activity - prevent...
- Plantar fascia
- Plantar fasciitis
- Posterior cruciate ligament...
- Posterior spinal anatomy
- Psoriasis - guttate on the ...
- Psoriasis - guttate on the cheek
- Radial head injury
- Radial nerve dysfunction
- Raynaud's phenomenon
- Reactive arthritis - view o...
- Retrocalcaneal bursitis
- Rheumatoid arthritis
- Rheumatoid arthritis
- Rheumatoid arthritis
- Rheumatoid arthritis
- Rotator cuff muscles
- Runners knee
- Sacrum
- Sciatic nerve
- Sciatic nerve damage
- Sclerodactyly
- Scoliosis
- Scoliosis
- Scoliosis brace
- Shin splints
- Shoulder arthroscopy
- Shoulder joint
- Shoulder joint inflammation
- Shoulder sling
- Signs of scoliosis
- Skeletal spine
- Skeleton
- Smashed fingers
- Spinal anatomy
- Spinal cord injury
- Spinal curves
- Spinal fusion
- Spinal stenosis
- Spinal stenosis
- Spinal tumor
- Spine supporting structures
- Sprained ankle
- Superficial anterior muscles
- Surface anatomy - normal palm
- Surface anatomy - normal wrist
- Synovial biopsy
- Synovial fluid
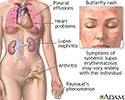
- Systemic lupus erythematosus
- Systemic lupus erythematosu...
- Tailbone (coccyx)
- Telangiectasia
- Tendinitis
- Tendon vs. ligament
- Tendonitis
- Tendons and muscles
- The structure of a joint
- Thigh stretch
- Tibial nerve
- Tophi gout in hand
- Torn lateral collateral ligament
- Torn medial collateral ligament
- Torticollis (wry neck)
- Treatment for leg strain
- Triangular shoulder sling
- Triceps stretch
- Ulnar nerve damage
- Uric acid crystals
- Vertebra, cervical (neck)
- Vertebra, lumbar (low back)
- Vertebra, thoracic (mid back)
- Vertebrae
- Vertebral column
- Vitamin D source
- Weight loss
- Whiplash
- Wrist anatomy
- Wrist splint
- X-ray
- X-ray
- Yo-yo dieting
Presentations
- Ankle sprain - Series
- Anterior cruciate ligament ...
- Bone fracture repair - series
- Bunion removal - series
- Carpal tunnel repair - series
- Clubfoot repair - series
- Creating a sling - series
- Hand splint - series
- Hip joint replacement - series
- Knee arthroscopy - series
- Knee joint replacement - series
- Leg lengthening - series
- Lumbar spinal surgery - series
- Microdiskectomy - series
- Partial knee replacement - ...
- Rotator cuff repair - series
- Shoulder separation - series
- Spinal bone graft - series
- Spinal fusion - series
- Spinal surgery - cervical -...
- Two person roll - series

 Bookmark
Bookmark